Knowing the warning signs and prevention for dental implant complications helps anyone considering implants make safer choices. This guide explains the most common implant problems, early red flags to watch for, practical steps to lower your risk, and what to do if you’re worried. Understanding these points can protect your health and your investment in a new smile.
Most common dental implant complications
Infection and peri-implantitis
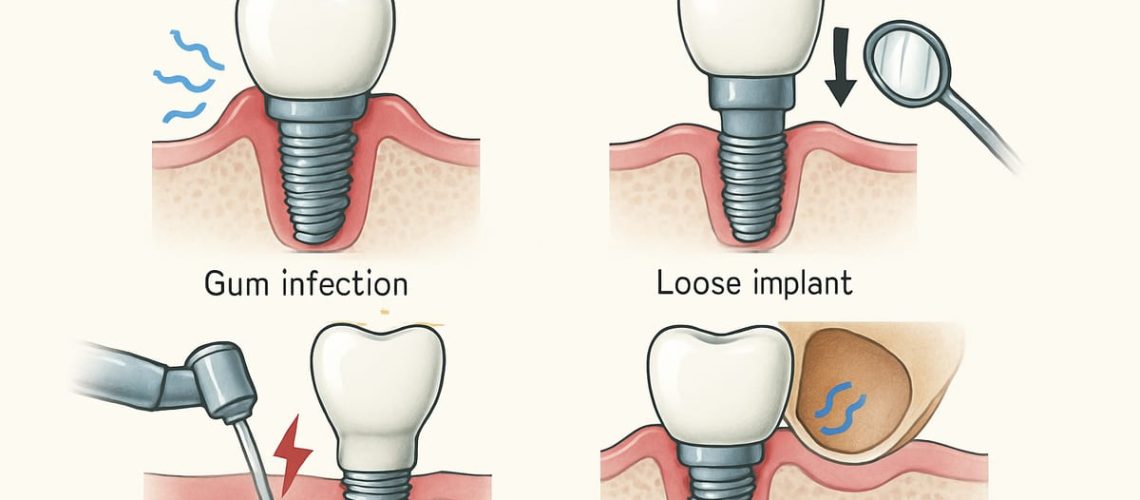
Peri-implantitis is a bacterial infection that attacks the soft tissue and bone around an implant. If untreated, it can cause bone loss and loosening of the implant. Symptoms include redness, swelling, bleeding gums, pus, and a bad taste or odor.
Failed osseointegration (implant failure)
Osseointegration is the process where the implant fuses with your jawbone. Failure happens when the implant does not bond properly. Common causes include poor bone quality, uncontrolled medical conditions, smoking, infection, and excessive early loading of the implant.
Nerve injury and altered sensation
Nerve injury can cause numbness, tingling, or a burning sensation in the lip, chin, gums, or tongue. This often happens when an implant is placed too close to a nerve or when swelling compresses a nerve. Some nerve issues are temporary; others can be long-lasting without prompt treatment.
Sinus or sinus membrane issues
Upper jaw implants near the sinus can perforate the sinus membrane, leading to chronic sinusitis or discomfort. Proper imaging and planning reduce this risk, and surgeons may perform a sinus lift or use longer implants positioned safely away from the sinus.
Prosthetic problems and mechanical failure
Problems with the crown, bridge, or screws include loose restorations, fractured screws, worn components, and poor fit. These mechanical issues can cause pain, chewing problems, or damage to the implant if not corrected quickly.
Early warning signs to watch for after implant surgery
- Severe or worsening pain after 48–72 hours
- Fever or chills
- Persistent or increasing swelling, redness, or drainage
- Loose implant or loose crown/prosthesis
- New or worsening numbness, tingling, or altered sensation
- Prolonged bleeding that won’t stop
- Persistent bad taste, odor, or difficulty chewing
If you notice any of these signs, contact your surgeon right away. Avoid poking or prodding the area, keep a log or photos of symptoms, and follow any emergency instructions from your surgical team.
How to reduce risk of dental implant complications
Comprehensive pre-op evaluation and planning
Thorough planning lowers risk. This includes a full medical history, medication review, and 3D imaging (CBCT) to check bone, nerves, and sinuses. Digital treatment planning helps select the right implant size and position before surgery.
Control medical risk factors
Manage chronic conditions like diabetes and discuss bone-health medications (for example, bisphosphonates) with your surgeon. Quit smoking at least several weeks before and after surgery—smoking greatly increases complication risk. Work with your doctor to optimize overall health before implants.
Good surgical technique and digital workflows
Using guided surgery and precise surgical techniques reduces chances of nerve or sinus injury and improves implant position for long-term success. Digital workflows, from intraoral scans to in-house lab fabrication, improve fit and reduce mechanical problems with the final prosthesis.
Post-op care and maintenance
Follow post-op instructions closely: soft diet as directed, prescribed antibiotics or rinses, and careful oral hygiene. Keep scheduled follow-ups so your team can catch inflammation or bone loss early. Treat gum inflammation promptly to prevent progression to peri-implantitis.
Choosing care and next steps if you’re worried
If you suspect a problem, seek a consult with a surgical implant specialist. Texas Center for Oral Surgery & Dental Implants is staffed by board-certified oral and maxillofacial surgeons who use advanced digital tools—X-Nav dynamic guidance, CBCT imaging, an in-house lab with zirconia milling and 3D printing, plus on-site sedation—to evaluate and treat complications.
At a consultation you can expect a focused exam, 3D imaging to assess bone, nerves, and the implant, and a clear treatment plan. Treatment may include antibiotics and cleaning, soft-tissue care, bone grafting, or a revision procedure if needed. The team will explain options, recovery expectations, and follow-up care.
If you notice warning signs or want a pre-op risk evaluation, contact the Texas Center for Oral Surgery & Dental Implants to schedule an assessment. Early action improves outcomes and helps protect your implant investment.